Who Is a Good Candidate for ICSI? Key Factors to Consider
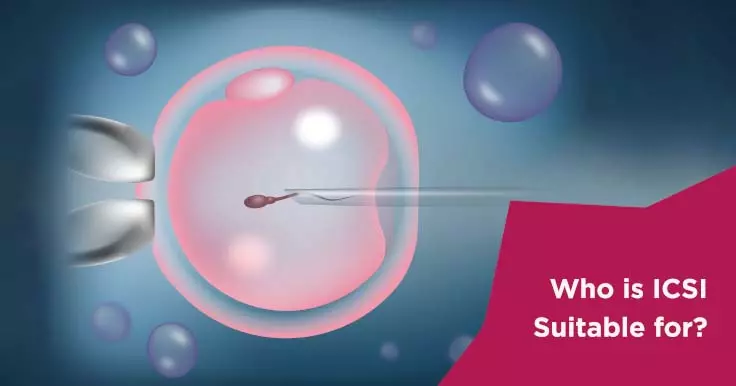
ICSI is a microscopic technique used to fertilize eggs with sperms. As opposed to conventional IVF, where the eggs and sperms are mixed in a petridish and left alone to fertilize on their own, in ICSI, each sperm is picked up under the microscope with the help of a needle and injected into each egg for fertilization.
Who is ICSI suitable for?
Conventional IVF requires the presence of a large number of sperms that can swim actively and are morphologically normal. For some couples, the number of available sperms may be too low for them to be able to actively swim up to an egg and fertilize it. They may be too weak to penetrate it. Or there may be other factors preventing fertilization, so for these couples IVF is not an option. However, ICSI provides hope in these circumstances.
The only step different between ICSI and IVF is the method of fertilization. As far as the patient is concerned, all the steps of the clinical part of the treatment are identical in both the procedures.
In what situations is ICSI recommended?
ICSI is recommended in situations where achieving fertilization may be difficult. These include:
- Low sperm counts
- Poor sperm motility
- High percentage of abnormal sperms
- When sperm has been extracted by electro-ejaculation
- In cases of azoospermia, where sperm has been surgically extracted directly from the epididymis (PESA) or testes (TESA/TESE)
- When there has been a previous fertilization failure or low rates of fertilized eggs after conventional IVF
- When using frozen oocytes
- Where there are less number of eggs available, such as poor responder women, to ensure better fertilization rates
Azoospermia is the complete absence of sperms from the ejaculated semen sample, that is, the sperm count is zero. It may be of two types: obstructive or non-obstructive. Obstructive azoospermia occurs due to a blockage that prevents sperms that are normally produced in the testes from coming out into the ejaculate. This may happen due to a previous vasectomy, due to congenital absence of the vas deferens, or due to infections in the past that may have caused scarring. In such cases, the chances of obtaining sperms via a PESA or TESA are good. However, as the sperms obtained are too few, ICSI is required. In cases of non-obstructive azoospermia, the testes fail to produce sperms. In some cases, sperm production may be present but too low. In such situations also there is a possibility of performing ICSI with sperms obtained surgically, though they may be absent in the ejaculate.
 Infertility Counselling
Infertility Counselling Female Infertility Treatment
Female Infertility Treatment Andrology Treatment
Andrology Treatment Fertility Enhancing Surgeries - Female
Fertility Enhancing Surgeries - Female Fertility Enhancing Surgeries - Male
Fertility Enhancing Surgeries - Male Endoscopy Treatment
Endoscopy Treatment IUI Treatment
IUI Treatment IVF Treatment
IVF Treatment ICSI Treatment
ICSI Treatment Advanced IVF Solutions
Advanced IVF Solutions Embryology
Embryology Vitrification Egg, Embryo, Sperm Freezing
Vitrification Egg, Embryo, Sperm Freezing Preimplantation Genetic Testing (PGT)
Preimplantation Genetic Testing (PGT) Donation Program Embryo / Egg / Sperm
Donation Program Embryo / Egg / Sperm Self-cycleTM IVF
Self-cycleTM IVF

 Self-cycleTM IVF
Self-cycleTM IVF