PCOS and Ovulation Induction: A Journey to Conception with Nova IVF

The couple had a wonderful married life for 7 to 8 years. However, when the couple wanted to start a family of their own, they discovered becoming parents turned out to be much more difficult than expected. The wife experienced unexpected changes, gaining weight (becoming obese) in a short time.
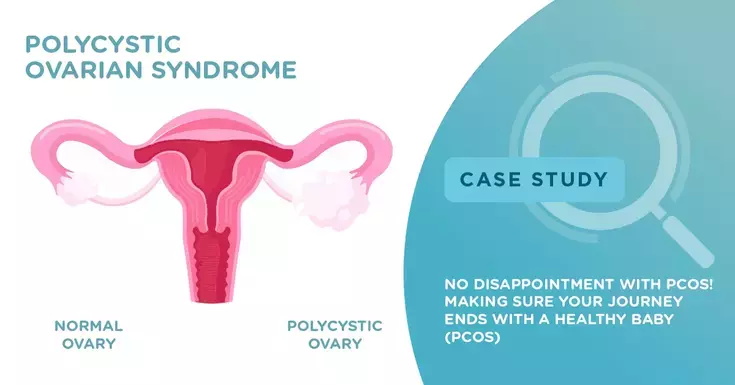
Struggling to Conceive with Polycystic Ovary Syndrome (PCOS)
After several months of trying to get pregnant on her own and some emotional visits to her gynecologist, the woman was diagnosed with PCOS, and she was referred to one of Nova IVF's fertility specialists, Dr. Yamini Agarwal.
The couple contacted Nova IVF Siliguri in West Bengal and made an appointment with Dr. Yamini Agarwal. The wife was advised to undergo diagnostic tests to rule out any other fertility problems, and as soon as the test results came in, Dr. Yamini Agarwal agreed that because of her PCOS, the wife would probably need a little assistance to conceive.
What is PCOS?
PCOS is a hormonal dysfunction that leads to multiple follicles within the ovaries, thus leading to anovulation (when the egg is not released) or ovulatory dysfunction (irregular ovulation) and causing manifestations of hyperandrogenism (excessive presence of androgens, the male sex hormones). The accumulation of follicles causes an overproduction of male hormones, which are usually present in small quantities in the female body.
The couple agreed on a treatment plan with Dr Yamini, deciding to start with In-Vitro Fertilisation (IVF) as she had history of failed ovulation inductions with medications and injections.
Ovulation Induction in Anovulatory Cycles
Ovulation induction is an assisted reproduction method to treat fertility problems in women who do not ovulate regularly or at all, because of PCOS.
What is Ovulation Induction?
Ovulation induction is a simple procedure that promotes ovulation. In women who do not ovulate at all, this pharmacological treatment aims to release a mature egg. Ovulation induction is often part of other treatments, such as In-Vitro Fertilization (IVF). The drugs administered stimulate the ovaries to increase the number of eggs released per cycle, to maximize the chances of conceiving during IVF.
Throughout this period, the wife underwent multiple ovulation inductions outside with letrozole (an oral medication commonly used to treat infertility in women suffering from ovulatory dysfunction or unexplained infertility) and low dose gonadotropin injections.
The wife had unilateral obstruction of the fallopian tubes (obstruction in only one tube), which further complicated the fertility process. Given these challenges, the wife and her partner proceeded with IVF with high doses of gonadotropins as the next step.
Injectable Gonadotropins
The administration of injectable gonadotropins was prescribed, which included daily injections of follicle stimulating hormone (FSH) for approximately 10 to 15 days to prompt the development of mature follicles.
During IVF, surprisingly, the wife had a poor response even with high doses of gonadotropins.
Despite the challenges, the coupled developed 4 follicles. On 3 day, 3 embryos were formed.
Embryo transfer is the final stage of the In-Vitro Fertilisation (IVF) process. If the fertility treatment has been successful, a positive pregnancy test 14 days later will confirm that pregnancy has finally been achieved. The choice of the day of embryo transfer depends on the number of embryos, their quality and patient's choice. The fertility specialist is to determine whether there are more advantages to transfer on day 3 or day 5 of embryo development.
Embryo Transfer on Day 3
In natural pregnancy, fertilisation takes place in the fallopian tubes and only on the 5th-6th day that the embryo reaches the uterus and is implanted in the endometrium. However, when trying to get pregnant with assisted reproduction, embryos are cultured in the laboratory in an environment mimicking female reproductive tract.
Advantages of Day 3 Transfer
The main advantage of early embryo transfer is that more embryos are likely to be available. As the days of culture in the laboratory pass, some embryos stop developing and therefore become unavailable. This is one of the reasons why some fertility specialists prefer to transfer on day 3, when the embryo has 6-8 cells. Thus, the risk of cancellation of the transfer is lower on day 3 than if the embryos remained in culture until day 5 or 6. In addition, another advantage is that the number of embryos to be vitrified is greater, and they can be used for future embryo transfers.
Of 3 embryos, 2 embryos were transferred into the uterus via embryo transfer. Fortunately, the wife conceived twins, although one turned out to be a blighted ovum (a type of miscarriage when an embryo stops growing), because of which the wife had only one ongoing pregnancy. This case shows that patients with PCOS are not always hyper responders; they can be poor responders too. This underscores the variability in how PCOs can manifest itself and influence infertility treatments.
 Infertility Counselling
Infertility Counselling Female Infertility Treatment
Female Infertility Treatment Andrology Treatment
Andrology Treatment Fertility Enhancing Surgeries - Female
Fertility Enhancing Surgeries - Female Fertility Enhancing Surgeries - Male
Fertility Enhancing Surgeries - Male Endoscopy Treatment
Endoscopy Treatment IUI Treatment
IUI Treatment IVF Treatment
IVF Treatment ICSI Treatment
ICSI Treatment Advanced IVF Solutions
Advanced IVF Solutions Embryology
Embryology Vitrification Egg, Embryo, Sperm Freezing
Vitrification Egg, Embryo, Sperm Freezing Preimplantation Genetic Testing (PGT)
Preimplantation Genetic Testing (PGT) Donation Program Embryo / Egg / Sperm
Donation Program Embryo / Egg / Sperm Self-cycleTM IVF
Self-cycleTM IVF

 Self-cycleTM IVF
Self-cycleTM IVF












Add new comment